by revityteam | Jun 19, 2024 | TMS Therapy Articles
If you have been grappling with panic disorder, you’re all too familiar with the rush of fear and overwhelming sensations that come with panic attacks.
It’s not merely about feeling anxious — panic disorder can seriously disrupt your daily life, making even the simplest tasks feel daunting. But the good news is that there are effective strategies out there that can help you manage and even prevent these intense episodes.
In this blog, we’ll explore some practical coping strategies for panic disorder. From immediate techniques to calm a panic attack to long-term approaches that reduce its frequency, we’ll cover a range of tactics you can start using today.
We’ll also discuss when it might be time to seek professional help and how building a strong support network can make a big difference in your journey toward recovery.
Whether you’re dealing with panic attacks yourself or supporting someone who is, understanding these strategies will empower you to regain control and lead a calmer, more fulfilling life. So, let’s get started and explore these techniques together!
What is panic disorder?
Imagine this: out of nowhere, you’re hit with an intense fear that ramps up within minutes into a full-blown panic attack. You might feel like you’re losing control, having a heart attack, or even like you’re dying. It’s way beyond the normal anxiety everyone experiences from time to time.
Panic disorder is when you have repeated episodes of these panic attacks, and you live in fear of when the next one will strike. It’s not only the attacks themselves but also the constant dread that another one could come at any moment. This can throw a wrench into daily life, making it hard to function at work, in social settings, or even when trying to relax at home.
Physically, during a panic attack, you might experience heart palpitations, sweating, trembling, shortness of breath, or a feeling of being smothered. Some people feel chest pain or discomfort, nausea, or dizziness. It’s often accompanied by a sense of detachment from the world or a fear of losing control.
What makes panic disorder particularly tough is the way it can make you start avoiding places or situations where you fear a panic attack might happen. This can lead to behaviors that limit your life.
The good news? It’s treatable. Therapies like cognitive behavioral therapy, medication, TMS therapy, and lifestyle changes help manage the symptoms and reduce the frequency of attacks. It’s all about finding the right combination that works for you.

Immediate techniques to halt panic attacks
Deep breathing exercises
Deep breathing is super effective because it helps counteract some of the physiological symptoms of a panic attack, like rapid heart rate and shallow breathing. Here’s a simple technique to try:
- Find a comfortable place to sit or lie down.
- Close your eyes and slowly inhale through your nose, counting to four. Focus on filling your lungs.
- Hold your breath for a count of four.
- Slowly exhale through your mouth for another count of four.
- Repeat this cycle five to ten times.
This method is called the 4-4-4 breathing technique. It helps regulate your breathing and induces a relaxation response in your body, cutting through the panic.
Grounding techniques
Grounding techniques are all about reconnecting with the present moment, which helps distract you from the overwhelming feelings and bring you back to reality. One popular method is the 5-4-3-2-1 technique:
- Acknowledge FIVE things you see around you. It could be a bird, a spot on the ceiling, or anything in your surroundings.
- Identify FOUR things you can touch around you. It could be your chair, the ground, or your own hair.
- Recognize THREE things you can hear. This could be any external noise, like a car passing by, birds chirping, or background noise.
- Notice TWO things you can smell. If you need to, walk nearby to find a scent.
- Acknowledge ONE thing you can taste. What does the inside of your mouth taste like — gum, coffee, or that sandwich from lunch?
This technique forces you to focus on your senses, which can effectively interrupt the escalating panic and help ground you in the here and now.
Visualization
Visualization or guided imagery involves mentally transporting yourself to a peaceful, calming place or situation to distract from the distress:
- Close your eyes, and take a couple of deep breaths to start relaxing.
- Picture a serene setting where you feel completely relaxed. This could be a beach, a favorite vacation spot, or a quiet forest.
- Imagine yourself there. What do you see around you? What sounds do you hear? Perhaps the gentle crash of ocean waves or birds in the trees? What scents are in the air? Feel the sun on your skin or the breeze in your hair.
- Immerse yourself in this place and allow yourself to feel calm and safe.
Visualization helps by engaging your mind in creating a calming and safe environment, which can take the edge off the panic until it passes.
These techniques aren’t merely useful; they’re powerful tools in your arsenal to manage panic attacks. Practice them regularly, even when you’re not experiencing a panic attack, so they become second nature when needed.

Long-term strategies to reduce occurrence
Cognitive Behavioral Therapy (CBT)
CBT is a cornerstone treatment for panic disorder because it addresses the thoughts and behaviors that trigger panic attacks. Here’s a deeper look at how it works:
| Identifying triggers |
Your therapist will help you recognize the situations and thoughts that provoke panic attacks. |
| Cognitive restructuring |
This involves challenging negative, panic-inducing thoughts and replacing them with more realistic, balanced perspectives. For example, if you tend to think, “I’m going to die” during a panic attack, CBT helps you learn to recognize this as a symptom of panic, not a prediction of actual harm. |
| Exposure therapy |
Gradually, and in a safe and controlled manner, you’ll face the fears you’ve been avoiding. This could start with imagining the feared situations and eventually build up to facing them in real life. |
| Skill development |
CBT also equips you with relaxation and visualization techniques to manage anxiety in the moment. |
By systematically breaking down and addressing these factors, CBT reduces the power that fear holds over you, diminishing the frequency and severity of panic attacks over time.
Medication
Medications often play a crucial role in managing panic disorder, especially when combined with therapy. Here are more details on the types commonly used:
Antidepressants
SSRIs (Selective Serotonin Reuptake Inhibitors) like Prozac or Zoloft and SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) like Effexor help by regulating neurotransmitters in the brain involved in mood and stress responses. It may take several weeks to notice their full effect.
Benzodiazepines
These are fast-acting anti-anxiety drugs that provide quick relief from acute symptoms of panic attacks. However, due to their addictive potential, they are generally prescribed only for short-term use or specific situations where quick anxiety relief is necessary.
While effective, these medications come with side effects like nausea, drowsiness, or dependency, so it’s important to have ongoing conversations with your healthcare provider about your treatment plan.
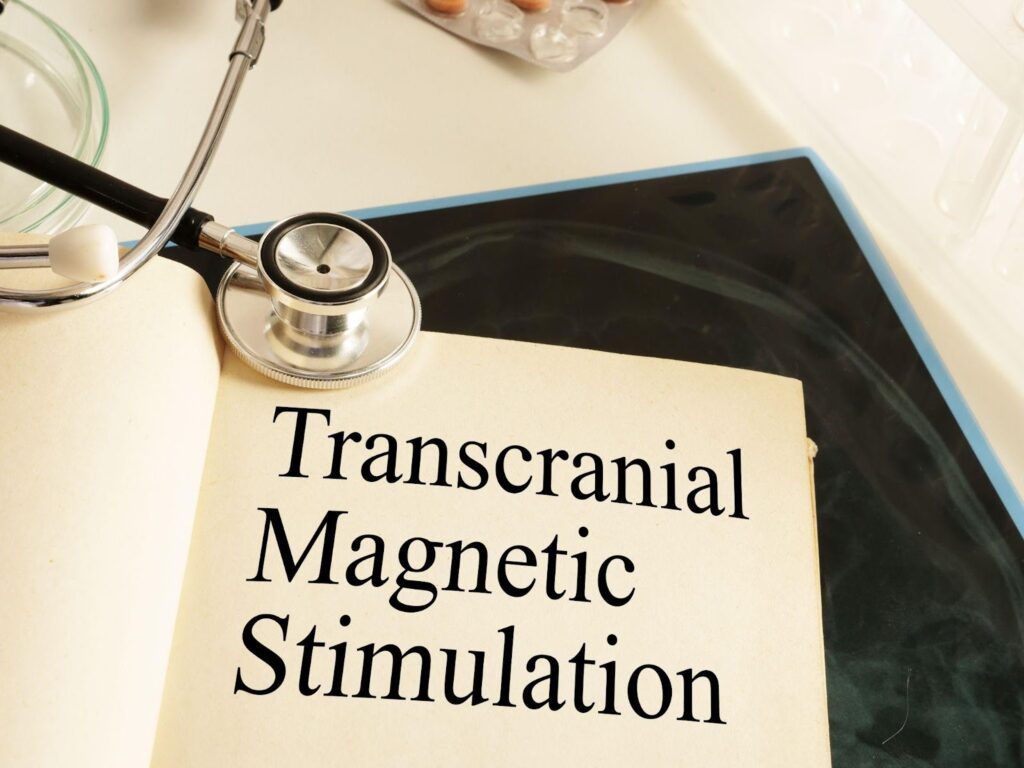
TMS therapy
Transcranial Magnetic Stimulation (TMS) offers a novel approach. During a TMS session, an electromagnetic coil is placed near your forehead. The device generates brief magnetic pulses, which stimulate nerve cells in the region of your brain responsible for mood control and anxiety.
A typical course of TMS for panic disorder might involve sessions 5 days a week for 4-6 weeks, but this can vary based on individual response.
For those who do not respond to medication or prefer a non-pharmacological approach, TMS can be an effective alternative. It has been shown to reduce symptoms of depression and is being studied for its effects on anxiety and panic disorders.
Lifestyle changes
Making specific lifestyle adjustments can significantly impact your ability to manage panic disorder.
Regular physical activity, particularly aerobic exercise, may help reduce the frequency and intensity of panic attacks by releasing endorphins and improving overall physical health.
Establishing a regular sleep schedule and creating a bedtime routine enhances sleep quality, which in turn reduces anxiety.
Eating balanced meals at regular intervals helps maintain blood sugar levels, which can mitigate mood swings and irritability. Reducing caffeine and sugar intake also helps decrease anxiety symptoms.
Practices like meditation, deep breathing exercises, and yoga increase your resilience to stress and provide tools to calm yourself during the onset of a panic attack.
By integrating these strategies into your daily life, you can manage the symptoms of panic disorder and enhance your overall mental and physical well-being. These approaches are not mutually exclusive and often work best when combined, offering a comprehensive approach to managing panic disorder effectively.

Building a support network
Building a strong support network is crucial when managing panic disorder. It provides you with emotional backing and enhances the effectiveness of other treatments. Here’s how you can establish and maintain a supportive environment:
Engage close friends and family
Start by opening up to your close friends and family. It’s important they understand what panic disorder entails and how they can support you during an attack. Educating them on the symptoms, triggers, and preferred ways to help you when experiencing a panic attack will help make a significant difference.
Professional support
Consistent communication with healthcare providers is essential. This could include therapists, counselors, and even your primary care doctor. They offer professional guidance, adjust treatments as necessary, and provide reassurance and support through your journey.
Support groups
Joining a support group is often incredibly beneficial. Connecting with others who are experiencing similar challenges provides a sense of belonging and reduces feelings of isolation. Support groups offer a platform to share personal experiences, coping strategies, and emotional support. These groups are invaluable, whether it’s a local in-person group or an online community.
Use digital tools
Numerous apps and online resources can connect you with support networks, provide quick coping mechanisms, and track your progress. Apps like mindfulness and meditation apps not only help in managing day-to-day anxiety but can also connect you with larger communities of people dealing with similar issues.
Create a safety plan
Collaborate with your support network to create a safety plan for when you feel a panic attack coming on. This plan can include who to contact, what strategies to implement, and what environment you need to feel safe. Having a plan can ease your mind and reassure you that you’re prepared to handle an attack effectively.
When to seek professional help
Let’s talk about when it might be time to consider getting professional help for your panic attacks. It’s important to recognize the signs indicating when a bit of extra support could be beneficial.
Frequent, intense panic attacks
If your panic attacks are happening so often that they’re disrupting your daily life — like affecting your job, your relationships, or your overall ability to function — it’s a clear sign that professional help could be necessary.
Fear of impending attacks
It’s also crucial to seek help if the fear of potential panic attacks starts controlling your actions. This could mean avoiding certain places, situations, or activities because you’re scared they might trigger an attack.
Physical symptoms overwhelm you
Panic attacks feel incredibly physical. If you’re experiencing symptoms that feel unmanageable or worried about your physical health during these attacks, it’s a good idea to consult a professional.
Limited success with self-help strategies
You might have tried several coping strategies on your own. However, if these aren’t helping or you find the panic attacks are still overpowering, a mental health professional can offer more structured treatment options like Cognitive Behavioral Therapy (CBT) medication or even recommend something like TMS therapy if traditional treatments aren’t working.
Impact on your mental health
Lastly, if you notice that your mental health is deteriorating — maybe you’re feeling more anxious in general, or you’re becoming depressed — it’s important to get professional support. These feelings can compound the stress you’re already experiencing from panic attacks and make everything feel a bit overwhelming.
Talking to a professional can provide you with tailored strategies and support to manage and reduce the frequency and severity of your panic attacks. They can help you get to the root of the issue and find effective, sustainable ways to cope.
Don’t hesitate to reach out — it’s like getting a check-up for any other part of your health. Remember, getting help is a sign of strength, not weakness, and it’s a proactive step towards taking control of your well-being.
TMS therapy at Brain Health Center
If you’re ready to explore a new path in managing your panic disorder, why not consider TMS therapy?
At Brain Health Center, we specialize in this innovative, non-invasive treatment that has shown promising results for many individuals struggling with panic attacks. Don’t let fear dictate your life any longer. Our experienced team supports you every step of the way, from initial consultation to tailored treatment plans.
Contact Brain Health Center today to learn more about how TMS therapy could be the turning point in your journey toward overcoming panic disorder. Take that first step towards a calmer, more controlled life.
by revityteam | Jun 12, 2024 | TMS Therapy Articles
Are you or someone you know grappling with ADHD and searching for the most effective treatment options? While medication has long been a staple in managing ADHD, TMS therapy has emerged as a compelling alternative, offering new hope to those seeking different solutions.
In this blog, we’ll dive deep into TMS therapy versus traditional medication, exploring the advantages, potential drawbacks, and overall effectiveness of each treatment.
Whether you were recently diagnosed with ADHD or are looking to enhance your current treatment plan, join us as we compare these two approaches to find out which might be the best fit for your needs.
Let’s start by looking at what ADHD is.

What is ADHD?
ADHD, or Attention Deficit Hyperactivity Disorder, isn’t merely about being restless or easily distracted. It’s a neurological condition that really dives deep into how someone thinks and acts, showing up as ongoing challenges with focus, hyperactivity, and impulsiveness.
People with ADHD might struggle to stay on task, get sidetracked easily, and often find it tough to manage what we call executive functions, like planning or decision-making.
You see this a lot in different age groups — kids, teens, and adults. For kids, it usually pops up as issues in school, like trouble following along in class or keeping up with homework.
Adults, on the other hand, might notice it more at work or in their personal lives, where staying organized and keeping on top of things feels a bit like juggling with too many balls in the air.
| Age Group |
Prevalence |
| Children |
5-7% |
| Adults |
2.5-5% |
Traditional ADHD medications
When it comes to tackling ADHD, the usual route involves two types of meds: stimulants and non-stimulants.
Stimulants, like methylphenidate (Ritalin, Concerta) and amphetamines (Adderall, Vyvanse), are pretty popular because they boost concentration and help dial down impulsivity and hyperactivity by upping neurotransmitter levels in the brain.
Then there are non-stimulant meds, such as atomoxetine (Strattera) and guanfacine (Intuniv). These are the go-to when someone doesn’t vibe well with stimulants or if they don’t do the trick. They work a bit differently but aim for similar results — easing those ADHD symptoms. Typically, these are the first treatments doctors consider.
The perks of these meds are pretty clear — they often really help improve focus, attention span, and self-control. But it’s not all smooth sailing; side effects range from the mild stuff like losing your appetite or feeling jittery to more serious issues like heart problems or the risk of dependency, especially with stimulants.
Going the medication route isn’t a decision to take lightly. It needs careful thought and regular check-ins with a doctor to keep everything on track. And remember, what works wonders for one person might not work for another — it’s all about finding the right fit for each individual.
Let’s take a closer look at each type of medication offered for ADHD so you get a sense of what to expect if you choose to take that route.

Stimulant medications for ADHD
1. Methylphenidate
Common brands: Ritalin, Concerta, Metadate
Upsides:
- Great for boosting focus and cutting down on fidgetiness.
- Helps control impulsive behaviors.
- Acts pretty fast, so you see results quickly.
Downsides and risks:
- Usual side effects include trouble sleeping, less appetite, headaches, and sometimes irritability.
- Might bump up heart rate and blood pressure.
- A risk of dependency, especially if misused.
- Long-term use in kids might affect growth.
2. Amphetamines
Common Brands: Adderall, Vyvanse
Upsides:
- Really sharpens concentration.
- Helps smooth out disruptive behaviors.
- Extended-release versions mean fewer doses throughout the day.
Downsides and risks:
- Similar side effects to methylphenidate, like sleep issues and decreased appetite.
- Might cause moodiness and a quicker heartbeat.
- Watch out for potential addiction.
- High doses might lead to serious heart-related issues.
3. Dextroamphetamine
Common Brands: Dexedrine
Upsides:
- Good for improving attention span.
- Helps dial down hyperactivity and impulsive acts.
- Might boost how well you organize tasks.
Downsides and risks:
- May reduce appetite, cause dry mouth, and lead to weight loss.
- Might feel a bit jittery or restless.
- High risk of abuse, particularly in adults.
- Long-term use sometimes causes heart complications.
4. Lisdexamfetamine
Common Brands: Vyvanse
Upsides:
- Designed to reduce abuse potential (needs to be processed in the body to activate).
- Keeps focus and attention steady throughout the day.
- You don’t have to take it as often because it lasts longer.
Downsides and risks:
- Possible side effects include less appetite, sleeplessness, and an uptick in heart rate.
- Might make you feel anxious or jittery.
- Lower abuse risk than other amphetamines but still something to be mindful of.
Non-stimulant medications for ADHD
1. Atomoxetine
Common Brand: Strattera
Upsides:
- Works differently from stimulants by specifically targeting norepinephrine levels in the brain, which helps increase attention and control impulsiveness.
- Doesn’t have the same abuse potential as stimulants, making it a solid choice for long-term use.
- Effective continuously throughout the day, so no need for multiple doses.
Downsides and Risks:
- Can cause nausea, fatigue, and mood swings, especially when starting the treatment.
- May increase heart rate and blood pressure, though generally less so than stimulants.
- Takes longer to see effects compared to stimulants — sometimes several weeks.

2. Guanfacine
Common Brands: Intuniv (extended-release), Tenex (short-acting)
Upsides:
- Often used for its ability to reduce hyperactivity and improve attention.
- May also help with reducing anxiety and improving sleep, which are sometimes issues for those with ADHD.
- Extended-release versions offer convenient once-a-day dosing.
Downsides and risks:
- Common side effects include drowsiness, fatigue, and, sometimes, headache.
- Sometimes causes a drop in blood pressure and a slow heart rate, which needs monitoring.
- Effects on cognitive improvement might be less pronounced than those seen with stimulants.
3. Bupropion
Common Brand: Wellbutrin
Upsides:
- Although primarily used as an antidepressant, it’s effective for ADHD due to its influence on dopamine and norepinephrine.
- Has a stimulant effect but with less potential for abuse.
- May improve mood and focus, which is a double win for those with coexisting depression.
Downsides and risks:
- Possible side effects include insomnia, headaches, and in rare cases, seizures.
- May not be as effective in managing all ADHD symptoms as the traditional stimulants.
- Interaction with other medications is a potential concern, requiring careful management.
4. Clonidine
Common Brand: Kapvay (extended-release), Catapres (short-acting)
Upsides:
- Particularly good at managing hyperactive and impulsive behavior.
- Can also be used to improve sleep, which is beneficial for individuals with ADHD who struggle with insomnia.
- The extended-release form allows for once-a-day dosing.
Downsides and risks:
- Sometimes leads to drowsiness, fatigue, and dizziness.
- Must be tapered off slowly to avoid withdrawal symptoms.
- May lower blood pressure and heart rate, requiring monitoring.
Non-stimulant medications provide valuable alternatives to stimulants, especially for individuals who may experience significant side effects or for whom stimulants are contraindicated. They typically have a lower risk of abuse and often address both ADHD symptoms and co-occurring conditions like anxiety or sleep disturbances.
However, they might not work as quickly or strongly as stimulants, so it’s important to have realistic expectations and closely work with a healthcare provider to find the most effective regimen.
Now that we’ve comprehensively studied the different medications available for ADHD patients, let’s look at the other half of the equation: TMS therapy.
An introduction to TMS therapy
Transcranial Magnetic Stimulation, or TMS therapy, is a noninvasive method that uses magnetic fields to zap nerve cells in the brain. It’s FDA-approved for treating depression, but lately, it’s getting a lot of buzz for helping with ADHD.
When you go in for a TMS session for ADHD, they place an electromagnetic coil pretty close to your head, right over what’s called the prefrontal cortex. That’s the part of your brain that handles attention and executive functions, which don’t always fire on all cylinders in folks with ADHD.
The treatment itself lasts about 4-6 weeks. During these sessions, the device sends repetitive magnetic pulses into the brain. It’s pretty chill — you stay awake and alert the whole time, and it’s generally comfortable.
The whole idea behind using TMS for ADHD is that it might help tune the brain’s activity levels. While researchers are still investigating this, early studies and trials are showing some promise. They suggest that it could really help enhance focus and dial down the hyperactive or impulsive behaviors that come with ADHD.
This table encapsulates the key attributes of TMS therapy:
| Feature |
Description |
| Type |
Non-invasive treatment |
| Target |
Prefrontal cortex of the brain |
| Mechanism |
Magnetic fields stimulate nerve cells |
| Session Duration |
It depends, based on the clinic you go to |
| Treatment Duration |
Typically 4-6 weeks |
| Condition Focus |
ADHD (also used for depression) |
| Research Status |
Emerging studies and ongoing clinical trials |
Comparing the effectiveness of TMS vs medication
So, when we’re comparing TMS therapy to medication for ADHD, it’s super important to look at the latest research and what’s actually happening in clinics.
As we’ve discussed, TMS therapy focuses on areas that handle mood regulation and executive functions, which are often a bit off in people with ADHD. It’s a newer approach, and there’s still more research to be done, but the results so far are pretty encouraging.
On the flip side, medications — both stimulants and non-stimulants — have been the go-to for ADHD for ages. The CDC says that these meds help reduce symptoms in about 70-80% of kids with ADHD. What’s more, the effects of stimulant meds kick in super fast, sometimes within an hour of taking it.
However, while medication acts quickly, you have to keep taking it to keep the symptoms at bay. TMS, though, might require several sessions spread over a few weeks to start seeing big improvements, but the benefits could last longer once you finish a full treatment course.
Choosing between TMS and meds isn’t about one being outright better than the other; it really comes down to what works best for the individual. It’s all about personal response to the treatment, what side effects someone might be willing to handle, and their preferences. Both are solid options and can be part of a tailored treatment plan.
| Treatment |
Efficacy |
Onset of Symptom Improvement |
Duration of Effectiveness |
| TMS Therapy |
Promising in recent studies |
Gradual, over weeks |
Potentially long-lasting after treatment course |
| Medication (Stimulants and Non-Stimulants) |
70-80% reduction in symptoms |
Rapid, often within an hour |
Ongoing use required |
Advantages and disadvantages of each treatment
So, when you’re weighing options for ADHD treatment, both TMS therapy and traditional medications have their pros and cons to think about.
Advantages of TMS therapy
Fewer side effects
TMS is non-invasive and really targeted, which means it generally has fewer side effects than medications. This is a big draw if you’re concerned about how meds might make you feel.
Non-invasive
It’s totally noninvasive, with no need for anesthesia or surgery, and you can jump right back into your day-to-day life after a session.
Disadvantages of TMS therapy
The main problem with TMS is that it’s not as easy to find as meds. It requires special equipment and trained personnel to administer, so it’s not available everywhere.
Advantages and disadvantages of medication
On the flip side, ADHD medications are pretty easy to get and are usually covered by insurance. But they come with their own bag of issues.
The side effects vary a lot from person to person, and figuring out the right medication and dosage is a process. Plus, there’s the worry about long-term effects like dependency or your body getting too used to the meds, which makes them less effective over time.
Choosing the right treatment really boils down to what fits best with your lifestyle, your body’s responses, and what you feel most comfortable with. It’s all about finding a balance that works for you.
| Treatment |
Advantages |
Disadvantages |
| TMS Therapy |
Fewer side effects, non-invasive |
Less accessible, potentially higher cost |
| Medication |
More accessible, often covered by insurance |
More side effects, concerns with long-term use |
Ultimately, neither treatment can be claimed as categorically superior; it is a matter of individual response and preference.
Try TMS therapy for your ADHD at Brain Health Center
Ready to explore a new avenue in your ADHD treatment journey? If you’re considering TMS therapy as an alternative or addition to your current treatment plan, Brain Health Center is here to guide you. Our expert team is equipped with the latest TMS technology and is deeply committed to providing personalized care that addresses your unique needs.
At Brain Health Center, we understand the challenges of ADHD and are dedicated to exploring innovative treatments that can make a real difference. TMS therapy offers a promising option with fewer side effects and a noninvasive approach. Don’t let traditional treatments be your only path — there may be another way to manage your symptoms more effectively.
Contact us today to schedule a consultation and learn more about how TMS therapy can fit into your overall ADHD management strategy. Let Brain Health Center help you take control of your ADHD, opening the door to improved focus and a better quality of life. Take the first step towards change — reach out now and see what TMS can do for you.
by revityteam | Jun 5, 2024 | TMS Therapy Articles
Brain mapping is an amazing tool that’s completely changing the game when it comes to understanding mental health disorders. It lets us see what’s going on inside the brain, giving researchers and clinicians a real-time view of its complexities. This technology is powerful for digging into the roots of various psychological conditions.
In this blog, we’ll explore how brain mapping broadens our understanding, making diagnoses more precise and treatments more personalized. It’s all about uncovering what’s hidden beneath the symptoms and advancing treatments tailored to individual needs.
From shining a light on the intricate mechanisms driving these disorders to leading the charge in developing targeted therapies, brain mapping is at the forefront of ushering in a new era in mental health care. Stick with me as we unpack the critical role this incredible technology plays in revolutionizing psychiatry and neurology.
What is brain mapping?
“What is brain mapping?” you may ask. Well, it’s the process of comprehensively studying the structure and function of the brain, allowing us to better grasp how it influences our thoughts, emotions, and behaviors.
By examining the brains of individuals with mental health disorders using brain mapping techniques, we can uncover valuable insights that pave the way for more effective treatment strategies.
There are several different kinds of brain mapping techniques. Let’s take a closer look.
Magnetic Resonance Imaging (MRI)
MRI is a widely used brain mapping technique that utilizes powerful magnets and radio waves to produce detailed images of the brain’s structure. With MRI, we’re able to visualize the various brain regions and identify any abnormalities or structural differences associated with mental health disorders.
By examining these structural variations, we correlate them with the symptoms and severity of different conditions, helping us tailor treatments to individual needs.
Positron Emission Tomography (PET)
PET scanning allows us to investigate the brain’s activity levels by injecting a radiotracer into the bloodstream. This radiotracer emits positrons, which the scanner detects and converts into images of brain function.
PET scans help identify areas of abnormal neuronal activity in mental health disorders. By pinpointing these regions, we gain a better understanding of how they contribute to specific symptoms and can develop targeted treatments accordingly.
Functional MRI (fMRI)
Next, we have fMRI, a technique that measures blood flow and oxygen levels in different brain areas, providing insights into brain activity. By comparing brain images taken during different cognitive tasks or emotional experiences, fMRI helps us understand how the brain’s functional networks contribute to mental health disorders.
This technique also allows us to examine how treatments and interventions affect brain function over time, aiding in developing more effective therapies.
Quantitative Electroencephalography (QEEG)
Now, let’s discuss the star of our discussion: QEEG. Using an EEG machine, this technique records your brain’s electrical activity by placing small sensors on the scalp. The data is then analyzed to identify patterns, frequencies, and deviations associated with mental health disorders.
QEEG provides valuable information about the brain’s functional connectivity and communication, giving us a unique perspective on how these disorders manifest.
What makes QEEG particularly exciting is its potential for individualized treatment. By examining the QEEG data of individuals with mental health disorders, we can identify specific brainwave patterns or imbalances that may contribute to their symptoms.
This enables us to develop personalized treatment plans, such as neurofeedback, which directly target these abnormal patterns and encourage healthier brain function.

How brain mapping helps us understand pathophysiology
Brain mapping is revolutionizing our understanding of mental health conditions. By looking at brain activity and connections, we’re starting to unravel the mysteries of how different disorders function at a neural level. This helps us see the complex networks involved in these conditions.
Let’s talk about depression, for example. With brain imaging, we’ve found that folks with depression often show unusual patterns in the prefrontal cortex, hippocampus, and amygdala — areas crucial for managing emotions, motivation, and memories. This helps us understand why symptoms like mood swings and memory issues arise in depression.
Then there’s something like schizophrenia. Imaging techniques like diffusion tensor imaging (DTI) have shown us how the white matter pathways, which help different brain areas communicate, are disrupted. These insights are crucial for grasping the underlying problems causing such a complex disorder.
One of the coolest parts of brain mapping is how it’s helping us find biomarkers for mental health issues. Biomarkers are measurable signs that indicate the presence of a disease, track its progress, or predict how well a treatment might work.
Although finding reliable biomarkers for mental health has been challenging, brain imaging is opening new doors here. We’re beginning to identify specific brain activity patterns that could help with early detection, choosing the right treatment, and monitoring how well that treatment is working.
For instance, research shows that cognitive-behavioral therapy (CBT) for anxiety can change how the amygdala and prefrontal cortex work, which we can see on brain scans, proving that the therapy is making a difference.
However, as exciting as brain mapping is, it’s not without its challenges. The technology is still evolving, and interpreting these brain images needs a careful, nuanced approach. We must remember that these images are only part of the story — they capture a moment in time and need to be considered alongside clinical assessments and observations.
Plus, mental health disorders are complex. It’s unlikely that brain mapping on its own will ever give us all the answers. Our understanding will keep growing as we integrate findings from genetics, neurobiology, and psychology.
So, while brain mapping is a powerful tool, it’s only one piece of the puzzle in understanding and treating mental health disorders.

Different disorders brain mapping helps with
Depression
You know how some days feel like you’re not in gear? Well, with depression, brain mapping has shown that this might be due to lower activity in the frontal lobes, the area that helps us manage emotions and make decisions.
Also, the amygdala, which handles emotional reactions, tends to be on overdrive. Understanding this helps tailor treatments like TMS to target these specific areas, making them more effective.
Anxiety
For those dealing with anxiety, it’s like their fear center, the amygdala, is always turned up to eleven. Brain mapping shows us this overactivity clearly, which is super useful. By pinpointing these hot spots, treatments can be designed to specifically calm these areas down, helping to alleviate those intense anxiety symptoms.
Bipolar Disorder
In bipolar disorder, brain mapping reveals a kind of activity rollercoaster in the brain that aligns with mood swings — from highs during manic episodes to lows in depressive states. This insight is crucial for developing treatments that aim to even out those extreme ups and downs.
Autism
With autism, brain mapping often shows us that there’s a different pattern in how brain regions connect and communicate, especially those that affect social skills. This is key for creating early interventions that can help improve social interactions and other related skills.
OCD (Obsessive-Compulsive Disorder)
For OCD, the brain’s habit loop, particularly in the orbitofrontal cortex, tends to be in overdrive. Mapping this out lets us target these areas with specific therapies like CBT or TMS to help break those compulsive routines effectively.
Panic Disorders
In panic disorders, it’s like the brain’s alarm system (again, the amygdala) is too sensitive, firing off panic when it doesn’t need to. Brain mapping helps us see this overactivity, guiding strategies to turn down the alarm system and reduce the severity and frequency of panic attacks.
Postpartum Depression
Postpartum depression will show up in brain maps as changes in areas tied to mood, empathy, and bonding. This insight guides us in helping new moms adjust better, managing symptoms that could affect their connection with their baby.
Insomnia
For insomnia, brain mapping might show us quirks in the parts of the brain that control sleep cycles. With this info, we can tailor interventions that specifically target these disturbances, hopefully leading to better sleep.
Brain mapping is like giving us a roadmap to the complexities of the brain involved in these conditions. It allows for more personalized and effective treatments. It’s fascinating stuff!

The future of brain mapping
Let’s chat about the really cool future of brain mapping. While we’ve come a long way with technologies like MRI, there’s still a ton of room to grow and refine these tools.
Researchers are constantly pushing the envelope, working to capture the brain’s activity in real-time, with sharper resolution and more precision. This could massively deepen our understanding of how the brain works and allow us to spot exactly where things go wrong in mental health disorders.
Imagine a future where doctors watch your brain’s activity unfold in real time, almost like streaming a movie! This could completely transform how we diagnose and treat mental health issues. We could zoom in on specific brain regions tied to disorders, making our treatments more personalized and spot-on.
Take anxiety or depression, for instance. With advanced imaging, we might be able to pinpoint the exact neural circuits involved and tailor treatments directly to those circuits based on your unique brain activity. This kind of precision could make treatments way more effective and cut down on the usual trial-and-error that goes with managing mental health conditions.
There’s also something exciting brewing at the intersection of genetics and brain mapping. As we better understand the human genome, we’re opening doors to new mental health explorations.
By merging genetic data with brain imaging, researchers could start to spot genetic markers that match up with specific brain irregularities. This blend of genetics and brain mapping could lead us to incredible breakthroughs, giving us clearer insights into how genetic variations influence mental health and paving the way for truly personalized treatment plans.
It’s an exciting time, and these advancements could be game-changers in our field!
Developing targeted therapies
The future of brain mapping holds promise for the development of targeted therapies. Currently, medications for mental health disorders often have a general effect on the brain, impacting various regions and neurotransmitter systems.
However, with the advancements in brain mapping, we envision more precise treatments that target specific dysfunctional brain circuits. This could reduce side effects and significantly improve symptom management — it’s like hitting the bullseye instead of shooting in the dark!
As we explore brain mapping further, addressing the ethical concerns associated with this emerging field is crucial. Privacy and informed consent are paramount when gathering intimate and sensitive data about an individual’s brain.
Striking a balance between advancing medical knowledge and respecting an individual’s autonomy and privacy will be a critical challenge as brain mapping research progresses.
Brain mapping at Brain Health Center
If you’re intrigued by brain mapping’s potential and its role in understanding and treating mental health disorders, consider experiencing this cutting-edge technology firsthand at Brain Health Center.
We’re excited to offer QEEG, a specialized form of brain mapping, absolutely free as a preliminary step before beginning TMS therapy. This unique opportunity allows you to see the direct benefits of advanced diagnostics in developing personalized treatment plans.
Don’t miss your chance to leverage these revolutionary tools in your journey toward better mental health. Contact Brain Health Center today to schedule your free QEEG session and discover how targeted TMS therapy makes a difference in your life.
Take the first step toward a deeper understanding of your brain’s function and unlock new possibilities for treatment.

by revityteam | May 22, 2024 | TMS Therapy Articles
Have you ever stopped to think about how much sleep impacts your overall quality of life and how a sleep center could help you improve yours? It’s about more than shutting down for a few hours — it’s a vital recharge that affects everything from your health to your mood to how you tackle your day.
Yet, for something so crucial, many of us struggle with getting the quality sleep we need. That’s where the magic of a sleep and wellness center comes into play.
In this blog, we’re exploring the transformative benefits of visiting a sleep and wellness center. Whether you’re battling insomnia, wrestling with sleep apnea, or trying to optimize your sleep patterns, these centers offer groundbreaking solutions.
From cutting-edge treatments like TMS therapy to comprehensive wellness programs that cover nutrition, stress management, and physical health, these centers are all about helping you achieve the best sleep of your life.
So, if you’re ready to elevate your well-being and transform how you feel every day, stick with me. We’re about to explore how these centers can improve your nights and change your days. Let’s get started on a journey to better sleep and a better life!
A comprehensive approach to sleep health
Getting your sleep right is absolutely crucial for feeling good and functioning well. Sleep isn’t “downtime” — it’s when your body and mind reboot and heal. But we get it, life moves fast, and sleep problems are pretty common, messing with both mental and physical health. That’s exactly why a sleep and wellness center could be a game-changer.
These places are goldmines because you get access to experts in sleep medicine. They’re not merely going to throw some pills your way and call it a day. They really dive deep, looking at how you sleep, your health history, and even how you live your day-to-day life to figure out exactly what’s throwing off your sleep.
With that information, they tailor a treatment plan for you. These centers are equipped with the latest tech to measure sleep quality accurately, so you know they’re not guessing what’s up.
One of the coolest treatments they offer is Transcranial Magnetic Stimulation or TMS. We’ll chat more about that soon, but it’s a standout therapy for sorting out sleep issues. Plus, these centers have a bunch of non-medication options to help get your sleep on track.
And it’s not all about zzz’s — these centers focus on overall wellness, too. They integrate stuff like diet, exercise, and stress management because it all ties back to how well you sleep.
Honestly, visiting a sleep and wellness center could totally revamp your sleep and, really, your overall well-being. You get a clear diagnosis, a treatment plan that’s all yours, and access to the latest therapies, all geared toward nailing down and tackling the root of your sleep problems.
Taking this step means setting yourself up for sharper thinking, better energy, improved mood, and a higher quality of life overall. Let’s dive deeper and see how these centers can help you take control of your sleep and feel better all around.
Access to advanced TMS therapy
One of the huge perks of visiting a sleep and wellness center is the access to top-notch TMS therapy. TMS therapy is this super cool, noninvasive technique where magnetic fields are used to zap specific parts of the brain. It’s seriously impressive and has been a game-changer for treating depression, anxiety, and even insomnia.
The centers are equipped with the latest and greatest equipment for this kind of therapy, which means you’re getting the most cutting-edge treatment.
If you’re wrestling with sleep issues and looking for some relief, this is a big deal because you know you’re getting the best care possible. It’s all about giving you that peace of mind that you’re in great hands and on the right path to sorting out your sleep.
Customized wellness programs
Let’s talk about these customized wellness programs they offer at dedicated centers. They’re really something because they tailor everything to fit your personal health needs, giving you the power to really take control of your overall well-being.
These programs cover everything you can think of — physical fitness, mental health, nutrition, managing stress, and sleep quality. One of the biggest wins here is gaining a deep understanding of your own body, which helps you make really informed choices about your health.
Now, let me break down some of the awesome benefits you get when you dive into a customized wellness program at a sleep center:
- Personalized approach: This is the real deal — you get a program that’s all about you. After some thorough assessments, the pros figure out your specific needs and craft a plan that targets exactly what you need to work on. This personal touch keeps you motivated and on track.
- Holistic approach: They look at everything, not only one part of your health. They understand how everything from your mental state to your physical health is connected. Adding things like yoga or meditation alongside regular fitness activities helps balance out every part of you.
- Targeted sleep solutions: If sleep issues are your nemesis, these centers are perfect. They specialize in sorting out sleep problems with things like TMS for insomnia, sleep hygiene practices, or relaxation techniques, which all help you get that much-needed restful night.
- Stress and mental health: We know life gets hectic, and these programs are designed to help you manage stress and bolster your mental health. They might include therapies or meditation practices that help clear your mind and strengthen your mental resilience.
- Nutrition and lifestyle: They also help you nail your nutrition game. You could get tips from nutritionists, personalized diet plans, or even cooking classes to help you eat better, which really changes how you feel day-to-day.
- Support and accountability: Going it alone can be tough, but with these programs, you’ve got a whole team. They keep you accountable, check in on your progress, and tweak things as needed to keep you moving towards your health goals.

Expert multidisciplinary teams
Imagine a group of highly specialized professionals from different fields, all working collaboratively towards a common goal — in this case, improving sleep health and overall wellness.
Sleep centers bring together experts from various disciplines to offer a comprehensive approach to addressing these interconnected factors.
So, who are the key members of an expert multidisciplinary team at a sleep and wellness center? Let’s take a closer look:
- Sleep specialists: These professionals are trained in diagnosing and treating sleep disorders. With their expertise, they can identify the underlying causes of sleep disturbances and design personalized treatment plans tailored to individual needs.
- Neurologists: These doctors specialize in disorders of the nervous system, including sleep-related neurological conditions. Their knowledge and experience are invaluable in assessing and managing conditions such as narcolepsy, restless leg syndrome, and sleep-related movement disorders.
- Psychologists: Sleep and mental health go hand in hand. Psychologists play a crucial role in addressing the psychological and emotional aspects of sleep disorders. They provide therapy, counseling, and cognitive-behavioral techniques, helping patients manage stress, anxiety, and other mental health challenges that may be impacting their sleep.
- Psychiatrists: For patients with sleep disorders related to psychiatric conditions like depression, anxiety, or bipolar disorder, psychiatrists offer specialized expertise. They can assess the need for medication, prescribe appropriate medications if necessary, and monitor the effects on sleep health.
- Nutritionists: Nutrition is an often overlooked aspect of sleep health. Nutritionists at these centers provide dietary counseling, helping patients optimize their eating habits to support better sleep patterns. They focus on nutrient-rich foods with sleep-inducing properties while also addressing any nutritional deficiencies that may be affecting sleep quality.
- Physical therapists: Sometimes, sleep disturbances are rooted in physical discomfort or pain. Physical therapists can evaluate musculoskeletal issues, provide targeted exercises, and recommend techniques to improve sleep posture and relieve pain. Their interventions can significantly reduce sleep disruptions caused by physical discomfort.
- Respiratory therapists: Sleep apnea is a common sleep disorder that requires specialized treatment. Respiratory therapists are experts in respiratory care and can provide continuous positive airway pressure (CPAP) therapy, ensuring adequate airflow during sleep for patients with sleep apnea.
Enhancing overall quality of life
We all want to boost our quality of life. We’re constantly hunting for ways to improve both our physical and mental health to really make the most of each day. Getting enough quality sleep is vital for our bodies. It’s when we’re asleep that our bodies repair themselves, our cells rejuvenate, our immune system gets a boost, and our tissues heal.
If you get solid, uninterrupted sleep regularly, you’ll have a stronger immune system, a lower risk of chronic diseases, and even a healthy weight. Sleep centers offer personalized advice and treatments to help you nail your sleep patterns and boost your physical health.
And it’s not only about the body — our brains need sleep, too. Quality sleep helps us think clearly, stay focused, and make smart decisions. Lack of sleep? It does the opposite: think brain fog, poor concentration, and slumping productivity.
By tackling sleep disorders head-on, these centers can help sharpen your cognitive functions and improve memory and overall mental performance.
One of the best things about these centers is how they handle sleep disorders like insomnia, sleep apnea, or narcolepsy, which can seriously mess up your sleep quality and leave you dragging all day. Without treatment, these issues can take a toll on both your physical and mental health.
At a sleep and wellness center, the experts will conduct thorough assessments to determine any sleep disorders you might have and then create a treatment plan tailored to your needs.
This might mean tweaking your lifestyle, some behavioral therapy, or maybe even trying something high-tech like TMS therapy.
TMS is a noninvasive technique in which magnetic fields stimulate parts of the brain involved in sleep regulation — pretty cool, right? It’s shown some promising results for people who haven’t had much luck with other treatments.
But, as we’ve discussed, it’s not all about sleep. These centers take a holistic approach, offering stress management, nutritional advice, and customized exercise plans—all designed to improve overall well-being by enhancing sleep quality.
So, investing time in visiting a sleep and wellness center is really an investment in your overall health. Getting professional help to sort out sleep issues will transform your sleep quality and seriously uplift various aspects of your life.
Whether you’re wrestling with a sleep disorder or simply want to optimize your sleep routine, these centers are a fantastic resource. Why not take control of your sleep and step up your quality of life starting today? Trust me, your body and mind will thank you!
Try TMS therapy at Brain Health Center
Ready to transform your sleep and elevate your overall well-being? If you’ve been struggling with sleep issues or want to optimize your sleep quality, it’s time to consider TMS therapy at Brain Health Center.
Our dedicated team uses the latest in TMS technology to help address various sleep-related disorders, providing personalized treatment plans that cater to your specific needs.
Don’t let another restless night affect your health and happiness. Contact Brain Health Center today to learn more about how TMS Therapy can make a profound difference in your life. Join the many others who have found relief and a renewed sense of vitality through our services. Your journey to better sleep and a healthier life starts here.

by revityteam | May 15, 2024 | TMS Therapy Articles
Let’s talk about something really important: postpartum depression. It’s way more severe than those typical “baby blues” that many new moms experience. It really throws a wrench into what should be a joyous time. It affects how moms bond with their babies and handle day-to-day life, and honestly, it’s quite tough.
In this guide, we’re diving into how Transcranial Magnetic Stimulation, or TMS, is helping to tackle PPD. It’s pretty groundbreaking and offers hope to those who haven’t had much luck with the usual treatments. We’ll explore how this innovative therapy works, why it might be a game-changer, and what it could mean for new moms struggling with these intense feelings.
Whether you’re going through this yourself, know someone who is, or simply want to understand more about postpartum depression, this guide is meant to provide insights and options. Let’s break down how TMS could help manage PPD and help moms enjoy this special time with their little ones.
Understanding postpartum depression
Postpartum depression (PPD) is a mood disorder that affects some women after childbirth. It goes beyond the commonly termed “baby blues” – which is a brief period of mood swings and anxiety following delivery.
PPD involves more severe and prolonged episodes of depression that may interfere with a mother’s ability to care for her child and handle other daily tasks.
Symptoms of PPD often include deep sadness, feelings of hopelessness, severe anxiety, loss of appetite, sleep disturbances, and sometimes even suicidal ideation.
Risk factors for PPD may include a history of depression, hormonal changes associated with childbirth, the stress of caring for a newborn, and insufficient support systems. Importantly, PPD is a diagnosable and treatable condition with the potential for full recovery.
Women with postpartum depression may experience a broad range of issues that affect their emotional and physical well-being, as well as their capacity for social interaction.
Signs of PPD typically appear within the first few weeks after giving birth, but they also manifest anytime during the first year postpartum. Recognizing and addressing these symptoms early is crucial for effective treatments and recovery.

What is TMS therapy?
Transcranial Magnetic Stimulation (TMS) is a noninvasive medical procedure that uses magnetic fields to stimulate nerve cells in the brain to alleviate depression symptoms. TMS therapy typically targets the prefrontal cortex, an area linked to mood regulation. Pretty cool, right?
During a TMS session, an electromagnetic coil is placed against the scalp near the forehead. This coil then emits short magnetic pulses that pass through the skull and induce small electrical currents, which stimulate nerve cells in the targeted brain region.
TMS therapy is generally considered an option for patients with treatment-resistant depression, meaning that they have not responded to traditional treatment options like antidepressant medication or psychotherapy.
One of the significant benefits of TMS is its minimal side effects, which usually are less severe than those of antidepressants. It is often recommended for individuals who cannot tolerate medication side effects or for whom medication isn’t advisable.
TMS sessions are typically conducted five times a week for four to six weeks. It’s FDA-approved for the treatment of depression and is also studied for other mental health disorders.
The efficacy of TMS in treating postpartum depression
TMS has emerged as a promising option for treating PPD. The efficacy of TMS is reflected in its ability to target the prefrontal cortex – an area often associated with mood regulation that is often underactive in depressive disorders. Research suggests that TMS improves depressive symptoms by stimulating neuronal activity in this region.
Here are some key points on TMS efficacy
- Targeted relief: Magnetic pulses directly influence the brain’s mood centers, offering precise treatment without systemic side effects.
- Improvement in symptoms: Many women with postpartum depression report a significant reduction in common symptoms such as depressed mood, sleep disturbances, and social interaction issues.
- Suitability for treatment-resistant cases: For those with a history of depression or those who don’t respond to antidepressant medication, TMS offers an alternative avenue for relief.
Therapeutic outcomes from TMS are supported by various studies, highlighting it as an effective treatment option, especially for those with treatment-resistant depression. While individual results vary, the non-invasive nature and targeted approach of TMS make it an attractive treatment for postpartum depression.
Benefits of TMS for postpartum depression
TMS presents several advantages when utilized as a treatment option for postpartum depression. Unlike conventional antidepressants, TMS has minimal side effects, making it a suitable alternative for nursing mothers concerned about medication infiltration into breast milk.
TMS uses noninvasive magnetic pulses to specifically target the prefrontal cortex, a brain region closely associated with mood regulation. This precision reduces the risk of unwanted systemic reactions.
Women with postpartum depression often notice improvements in mood, increased capacity for social interaction, and better sleep patterns.
The reduction of symptoms such as depressed mood and suicidal ideation indicates TMS’s potential as an essential tool within the spectrum of effective treatments for depression.
| Benefits of TMS |
Description |
| Minimal Side Effects |
Fewer systemic side effects compared to medications |
| Targeted Treatment |
Focuses on the prefrontal cortex to alleviate mood disorders |
| Efficacy |
Addresses depressive symptoms, including treatment-resistant cases |
| Improves Daily Functioning |
Enhances mood, sleep, and social interactions without requiring downtime |
This therapy empowers mothers to engage more fully in the formative moments of motherhood without the burdensome cloud of postpartum depression.
Insurance and cost considerations
Navigating the financial aspects of any treatment, including TMS therapy, is important for many patients and their families, especially when you’re adapting to life with a newborn.
Understanding the cost implications and insurance coverage options for TMS therapy helps ease the stress often associated with seeking treatment, especially for conditions like postpartum depression.
When it comes to sorting out the finances for TMS therapy, it can be a bit of a maze, especially with something as specialized as treating postpartum depression. Let’s break it down so you have a clear picture of what to expect and how to manage it.

Cost of TMS therapy
The price tag for TMS varies greatly depending on where you live, which clinic you go to, and the specific treatment plan. Typically, a complete course of TMS might require you to commit to several sessions each week over a few weeks.
Insurance coverage
Luckily, more insurance companies are starting to cover TMS, especially for major depression, but coverage for postpartum depression specifically might still be a grey area. The best move is to call your insurer directly and get the lowdown on what they’ll cover. Make sure to ask:
- Do they cover TMS for postpartum depression?
- Is there a limit on the number of sessions or a cap on how much they’ll pay?
- What kind of documentation do they need to approve the treatment?
Medicaid and Medicare
If you’re on Medicaid or Medicare, coverage for TMS may vary by state and plan. It’s worth making a call to your local office to see what’s covered and what the eligibility criteria are.
Out-of-pocket and financing options
If insurance won’t cover everything or you don’t have coverage, many clinics offer payment plans or scale their fees based on your income. There are also credit lines available specifically for healthcare expenses not covered by insurance, which could be a good option.
Discussing all this upfront will help you navigate the costs associated with TMS so that finances don’t stand in the way of getting the help you need.
Frequently asked questions
What exactly is postpartum depression?
Think of postpartum depression as a significant emotional and mental challenge that hits after having a baby. It’s way more intense than the baby blues, which are pretty common and pass quickly. PPD sticks around and really messes with a new mom’s ability to handle daily life, making it hard to care for herself and the baby.
It’s the last thing any mom wants to deal with while she’s already adjusting to motherhood or transitioning to life with another child.
How does postpartum depression differ from the ‘baby blues’?
Baby blues are like a brief storm of emotions that many new moms experience right after childbirth — think mood swings and weepiness that fade after a couple of weeks. Postpartum depression, though, is like a heavier, longer-lasting storm that really weighs you down and doesn’t go away as quickly or easily.
What does postpartum depression feel like?
Symptoms often include feeling really sad, empty, or hopeless, and sometimes being anxious to the point of panic attacks. There might be trouble bonding with the baby, feeling withdrawn, or even thoughts of harming oneself or the baby. It also often comes with big changes in appetite and sleep.
What causes this to happen?
There’s no single reason why PPD hits, but it’s likely a mix of hormonal changes after childbirth, the sheer exhaustion from delivery, emotional factors like adjusting to motherhood, and often, not having enough support.
Who is more likely to get postpartum depression?
It honestly happens to any new mom, but some things might up the risk, like a past history of depression, a family history of mental health issues, stressful life events, or not feeling supported.
What are the treatment options for postpartum depression?
Treatment typically involves therapy — things like talking it out with a counselor or cognitive-behavioral therapy. Medications also play a role, especially if the depression is severe. Sometimes, joining a support group where other moms share their experiences is really helpful too.
Can postpartum depression affect the baby too?
Yeah, it can. It might make bonding with the baby tougher, which affects the baby’s development and emotional health. However, with the right treatment and support, mothers manage PPD effectively and build strong, healthy relationships with their children.
How can loved ones help a mom dealing with postpartum depression?
Family and friends are super important here. They listen without judging, help out around the house, take care of the baby to give mom a break, and really encourage her to get professional help if things don’t seem to be getting better.
Is TMS therapy safe for nursing mothers?
Yes, TMS therapy is considered safe for nursing mothers. This makes it a suitable option for mothers who are breastfeeding and are concerned about the potential effects of traditional antidepressants.
Can TMS therapy be used as a standalone treatment for PPD?
TMS is an effective standalone treatment for some women with postpartum depression, especially those who prefer not to use medication or have not found medications effective. However, it is also part of a comprehensive treatment plan that includes therapy, counseling, and support groups.
What are the potential side effects of TMS therapy?
TMS therapy is generally well-tolerated. The most common side effects are mild to moderate headache and scalp discomfort during treatment sessions. These symptoms typically improve after the initial sessions as the body adjusts to the treatment. Severe side effects are rare but may include seizures. However, the risk is extremely low.
How do I know if TMS is the right treatment for my postpartum depression?
Deciding on the right treatment involves a thorough evaluation by a healthcare provider specializing in mental health and, ideally, postpartum issues. They will assess your medical history, severity of symptoms, and previous treatment responses.
If you’ve struggled with traditional treatments or are looking for a non-medication-based therapy, TMS might be a suitable option.
What should I expect during a TMS session?
During a TMS session, you will sit in a comfortable chair, and a small, curved device will be positioned over your head. This device generates magnetic pulses that stimulate specific parts of the brain associated with mood regulation. Each session lasts about 30 to 60 minutes, during which you can relax, listen to music, or watch TV.
Can postpartum depression return after successful TMS treatment?
As with other treatments for depression, there is always a possibility that symptoms return. However, many patients experience long-lasting relief after completing a course of TMS therapy. For those who notice symptoms reemerging, additional TMS sessions are scheduled to manage the symptoms effectively.
TMS therapy for postpartum depression at Brain Health Center
If you or someone you know is navigating the challenging waters of postpartum depression, it’s crucial to know that help is available and recovery is possible.
At Brain Health Center, we specialize in innovative treatments like Transcranial Magnetic Stimulation (TMS), which has shown promising results in treating postpartum depression. Our compassionate team is dedicated to providing support and effective care tailored to the unique needs of new mothers.
Don’t let postpartum depression overshadow the joy of motherhood. Reach out to us at Brain Health Center to explore how TMS therapy makse a significant difference. We’re here to help guide you through recovery with the most advanced care options.
Take the first step towards healing by contacting us today. Your well-being is our priority, and together, we will find the path back to enjoying this precious time with your baby.